by Visivo | Jan 16, 2020 | Uncategorized
You may be wondering why your Summit Family Care Dental office is choosing to talk about heart health. As a dedicated member of your medical team, we’re not only concerned with keeping your teeth and gums healthy, but rather we’re committed to keeping your whole body healthy. And it just so happens that your oral health plays a key role in overall wellness, including heart health. So during this American Heart Health Month, we want to provide all of our patients with important information on how keeping your smile in tip-top shape can help you maintain a healthy body.
How Does Dentistry Play a Role?
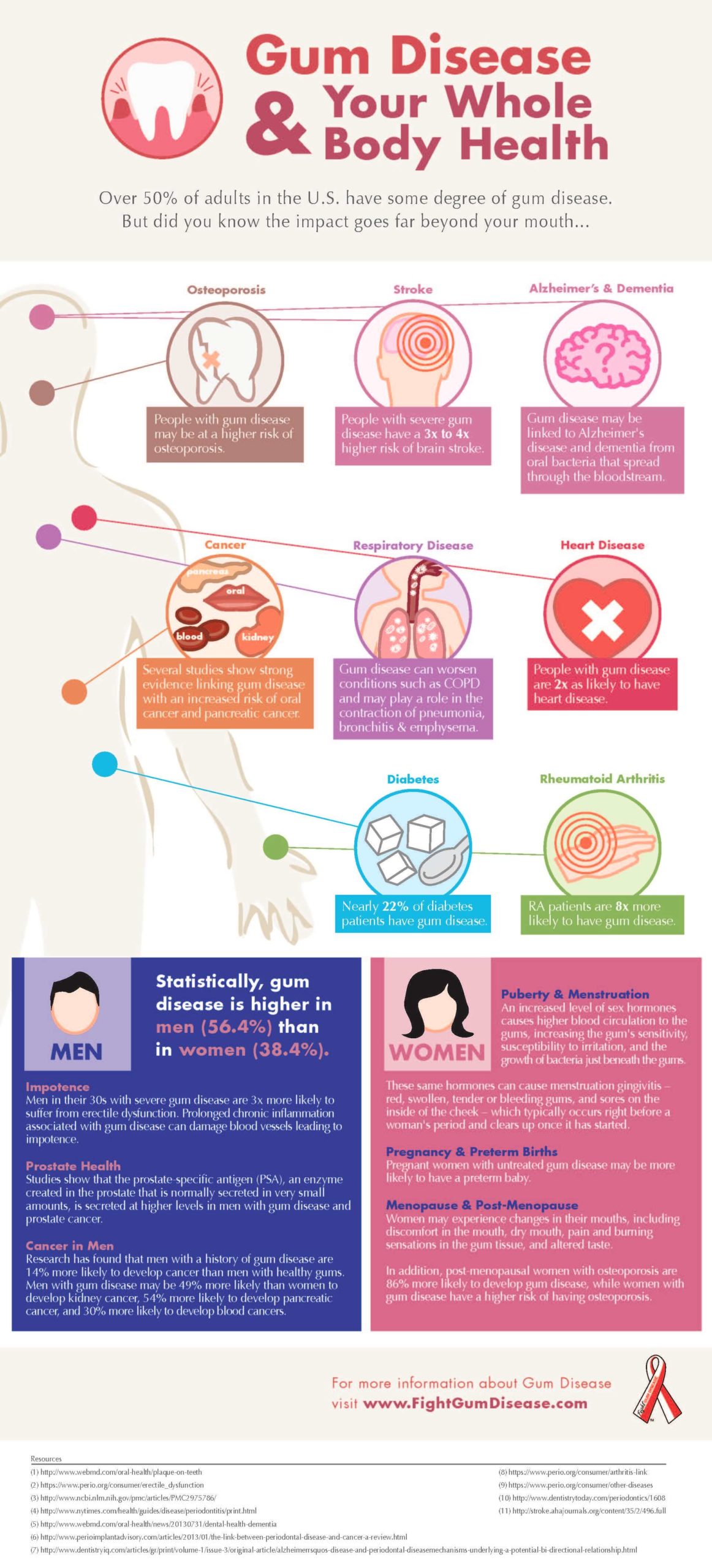
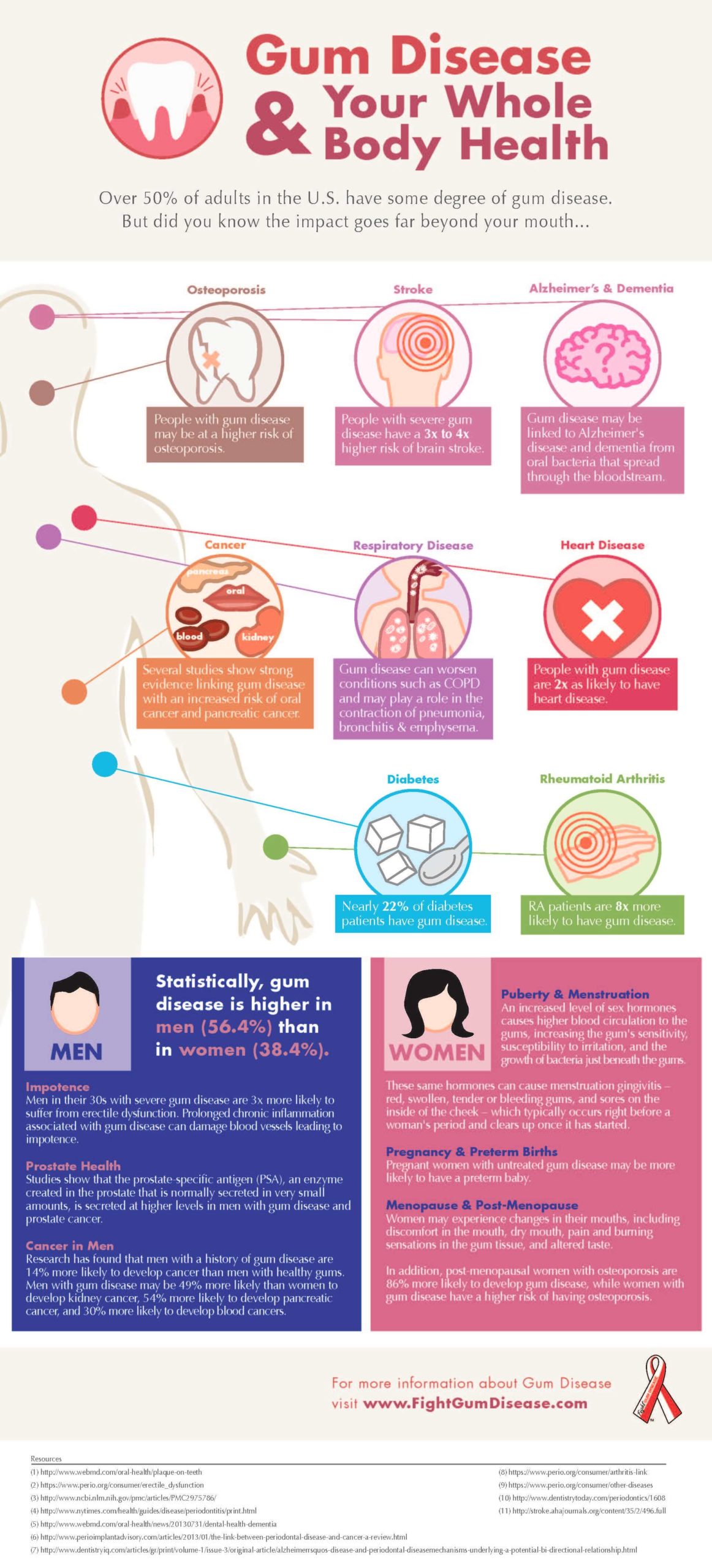
As research continues to advance what we know about heart disease, a strong correlation between oral health and heart health has been discovered. This link begins with gum health and, more specifically, gum disease. Gum disease is essentially an infection in the gum tissue that can lead to tooth loss. But perhaps what’s more concerning is that this infection has a direct route to the bloodstream. If it spreads, your body will produce excessive amounts of C-reactive protein (CRP), which is one of the known indicators of cardiovascular disease. Elevated levels of CRP can lead to some serious health issues including:
Inflamed arteries
Blood clots
Heart attacks
Strokes
How to Avoid Gum Disease
The best way to avoid gum disease and the dangerous effects it can have on your heart is to prevent it by brushing and flossing your teeth regularly. It’s also crucial to visit your dentist twice a year to remove buildup that your toothbrush just can’t touch.
Know the Signs
One of the scariest things about gum disease is that it can develop rapidly before you even suspect a problem. It is treatable and success is more likely if caught in the early stages. Knowing this, you should be aware of some early signs of gum disease so that you can seek treatment early. Some things to look out for include:
Bleeding when brushing or flossing
Puffy, tender gums
Bad breath
Teeth that feel loose
If you recognize any of the signs above, or it’s been more than six months since your last dental cleaning, call our dental office in Warsaw or Geneseo to schedule an appointment. Your smile and your heart will thank you.

by Visivo | Jan 16, 2020 | Uncategorized

by Visivo | Dec 30, 2019 | Uncategorized
It’s increasingly common to hear that oral health is vital for overall health. More than 80 percent of Americans, for example, are living with periodontal or gum disease, which often goes undiagnosed. This may be because the patient’s teeth feel fine, so he avoids going to the dentist, and visits to the physician rarely focus on oral health.
According to Delta Dental, however, there is now evidence of two specific links between oral health and heart disease. First, recent studies show that if you have gum disease in a moderate or advanced stage, you’re at greater risk for heart disease than someone with healthy gums. And second, your oral health can provide doctors with warning signs for a range of diseases and conditions, including those in the heart.
Why Are These Things Related?
Oral health and heart disease are connected by the spread of bacteria – and other germs – from your mouth to other parts of your body through the blood stream. When these bacteria reach the heart, they can attach themselves to any damaged area and cause inflammation. This can result in illnesses such as endocarditis, an infection of the inner lining of the heart, according to Mayo Clinic. Other cardiovascular conditions such as atherosclerosis (clogged arteries) and stroke have also been linked to inflammation caused by oral bacteria, according to the American Heart Association.
Who Is at Risk?
Patients with chronic gum conditions such as gingivitis or advanced periodontal disease have the highest risk for heart disease caused by poor oral health, particularly if it remains undiagnosed and unmanaged. The bacteria that are associated with gum infection are in the mouth and can enter the blood stream, where they attach to the blood vessels and increase your risk to cardiovascular disease. Even if you don’t have noticeable gum inflammation, however, inadequate oral hygiene and accumulated plaque puts you at risk for gum disease. The bacteria can also migrate into your bloodstream causing elevated C-reactive protein, which is a marker for inflammation in the blood vessels. This can increase your risk of heart disease and stroke, according to the Cleveland Clinic.
Symptoms and Warning Signs
According to the American Association of Periodontology (AAP), you may have gum disease, even if it’s in its early stages, if:
your gums are red, swollen and sore to the touch.
your gums bleed when you eat, brush or floss.
you see pus or other signs of infection around the gums and teeth.
your gums look as if they are “pulling away” from the teeth.
you frequently have bad breath or notice a bad taste in your mouth.
or some of your teeth are loose, or feel as if they are moving away from the other teeth.
Prevention Measures
Good oral hygiene and regular dental examinations are the best way to protect yourself against the development of gum disease. The American Dental Association (ADA) Mouth Healthy site recommends brushing your teeth twice a day with a soft-bristled brush that fits your mouth comfortably, so it reaches every tooth surface adequately. It also recommends that you use an ADA-accepted toothpaste such as Colgate Total® Advanced, which is proven to increase gum health in four weeks. You should also floss daily and visit your dentist for regular professional cleanings.
By being proactive about your oral health, you can protect yourself from developing a connection between oral health and heart disease, and keep your smile healthy, clean and beautiful throughout your life.
This article is intended to promote understanding of and knowledge about general oral health topics. It is not intended to be a substitute for professional advice, diagnosis or treatment. Always seek the advice of your dentist or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment.

by Visivo | Dec 30, 2019 | Uncategorized
You take your child to his dental appointment, expecting smiles all around and a clean bill of health. Instead, you discover that your child’s teeth are in a perilous state of decay, and your child will need thousands of dollars of dental work. You’re a good mom; you brush his teeth and feed him healthy foods. How could this happen?
The answer may be acid reflux. A study from the University of California at San Francisco found that children with reflux are six times more likely to suffer damage to the enamel than healthy children.
As children grow, their reflux medication may stop working. Many children go off their medication around age one, just when teeth are popping up. But some older children still have problems with reflux. A child may think that reflux is normal, and forget to mention it to you. Fortunately, there are steps you can take to minimize the consequences of acid reflux.
See the Dentist Early and Often
If your child has a history of reflux, make sure he sees the dentist as soon as he has teeth. A good pediatric dentist can spot reflux damage in its early stages and help you develop a treatment plan. Some children with severe acid reflux may need to see the dentist every three months instead of every six months. When you are dealing with acid damage, prevention is much more economical than waiting for a crisis.
Two, Four, Six, Eight—You Have Got to Fluoridate!
All children need fluoride, but it is especially important for children with acid reflux. Because their teeth are constantly under attack, they need the extra protection fluoride provides. If possible, encourage your child to drink fluoridated water. That way, he will get his fluoride throughout the day. If you have a well or use a water filter that removes fluoride from the water, talk to your dentist or pediatrician. You can get a prescription for liquid fluoride or fluoride pills.
Watch That Diet
For children with reflux, it is not enough to avoid sugary drinks and snacks. If you want to protect your child’s teeth, you need to reduce the flow of acid into the mouth. Avoid typical reflux trigger foods, such as tomatoes and other acidic fruits. Watch your child’s snacking schedule; avoid food right before nap time or bedtime. Finally, talk to your pediatrician to make sure you are doing everything possible to control reflux.
Baby teeth are important. They help your child get adequate nutrition and pave the way for adult teeth. If your child has acid reflux, you need to stay on top of his dental care. Your actions now could impact his future oral health.
This article is intended to promote understanding of and knowledge about general oral health topics. It is not intended to be a substitute for professional advice, diagnosis or treatment. Always seek the advice of your dentist or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment.

by Visivo | Oct 8, 2019 | Uncategorized
Types of Tooth Discoloration (Stains)
Tooth discoloration can occur as a result of surface stains, due to actual changes in your tooth material, or because of a combination of both factors. Dental professionals have identified three main categories of tooth discoloration:
- Extrinsic Teeth Stains: An extrinsic tooth stain is staining on the surface of the tooth. It occurs when stain particles, such as pigmented residue from food or drink, build-up in the film of protein that covers the tooth enamel. Extrinsic tooth stains are typically caused by tobacco use or by regularly drinking coffee and tea, wine or cola drinks. This type of tooth stain responds well to regular dental cleaning and brushing the teeth with whitening toothpaste.
- Intrinsic Teeth Stains: An intrinsic tooth stain is staining below the surface of the tooth. It occurs when stain-causing particles work through the exterior of the tooth and accumulate within the tooth enamel. Excessive fluoride use and also have been associated with intrinsic, especially in children. An intrinsic tooth stain is trickier to remove, but it can be done. An intrinsic tooth stain may require bleaching using professional or at-home chemical teeth-whitening products, such as Whitestrips.
- Age-Related Teeth Stains: Age-related teeth stains combine the results of both intrinsic and extrinsic tooth discoloration. Because the core tissue of your teeth, the dentin, naturally yellows over time, teeth discolor with age. As we age, the enamel that covers the tooth becomes thinner, allowing the dentin to show through. These intrinsic causes of discoloration combined with extrinsic causes such as the effects of certain foods, beverages, and tobacco, will cause most adults’ teeth to discolor with age.
Stained Teeth Causes
Teeth stains have many causes. Certain foods and drinks can cause teeth stains, and as we’ve talked about, tooth discoloration is also a product of several biological factors, including the transparency of your tooth enamel.
There are many causes of discolored teeth—some of which could have possibly been prevented, and many of which are beyond your control. This comprehensive list can help you determine the cause of discolored teeth, and in many cases, help prevent further discoloring of your teeth:
- Food & Drink: Coffee, tea, dark sodas, red wine, and even a few fruits and vegetables are proven causes of discolored teeth.
- Tobacco: Both cigarettes and chewing tobacco can contribute to discolored teeth.
- Oral Care: Poor dental hygiene, such as inadequate brushing or flossing, can lead to tooth discoloration.
- Trauma or Disease: Any trauma, illness, or disease that affects enamel development in children—either in the womb or while teeth are developing (under the age of 8)—can cause discolored teeth. Trauma to adult teeth can also cause discolored teeth. In addition, there are a few diseases and disease treatments that can cause discolored teeth. Chemotherapy and radiation, for example, discolor teeth.
- Medical Treatments: Sometimes medical treatments can contribute to teeth stain, and several classes of medications including high blood pressure medications, chemotherapy, antihistamines and some antipsychotic medications can cause teeth stains.
To know how to remove a tooth stain, it helps to know what type of stain you are dealing with. Paul A. Sagel, a Procter & Gamble Research Fellow, has conducted extensive research into the science of tooth stains. Research by Sagel and others have shown that some stain particles remain on the tooth enamel, while others work through the tooth enamel over time and set beneath the tooth surface, which creates dullness and tooth stain.
Are My Teeth White?
Tooth color is subjective, and it can be hard to tell how well teeth-whitening products are working to remove or reduce teeth stains. A 2004 study in the Journal of Dentistry showed that even professionals disagree on tooth color when evaluating the same teeth, and a single professional can rate the whiteness of the same tooth differently on different occasions. One method of evaluating the effectiveness of whitening products involves taking high-resolution digital images of teeth and assigning numerical values to describe the whitening effects three ways: a decrease in yellowness, decrease in redness, and an increase in lightness.
Teeth Whitening for Older Adults
While everyone knows you get better with age, tooth stains are one of the least-favorite body changes that take place during the aging process. In fact, one of the three main categories of tooth discoloration is age-related discoloration, which is a result of several factors.
Why Are Seniors Susceptible For Tooth Stains?
First, as you age, the outer layer of the tooth’s enamel gets thinner over time, revealing the natural yellow color of the core tissue of your teeth, called the dentin. This dentin also yellows naturally with age. In addition, years of drinking tea, coffee, dark sodas, and wine can cause progressive tooth stains over time. Finally, damage or injuries to your teeth, which occur over time throughout your life, cause discoloration that can become noticeable with age.
How to Remove Teeth Stains
Fortunately, there are many treatment options for teeth stains. Keep your teeth healthy and looking great by maintaining a consistent oral health routine including twice-daily toothbrushing and daily flossing, twice-yearly visits to your dentist, and by limiting your consumption of teeth-staining beverages. Regular whitening maintenance will help keep them looking whiter and brighter.
Regardless of the type of tooth discoloration you have, there are many safe, over-the-counter, teeth-whitening products available to help you makeover your discolored teeth into a beautiful white smile. Ask your dentist for recommendations on the best teeth whitening option to treat your age-related tooth stains and discoloration.
Sources:
- Vogel R. Intrinsic and extrinsic discolouration of the dentition: A review. Journal of Oral Medicine 1975;30:99-104
- Joiner A. Tooth colour: a review of the literature. Journal of Dentistry 2004;323-12
- Watts A, Addy M. Tooth discoloration and staining: a review of the literature. British Dental Journal 2001;190:309-316
- Gerlach RW, Zhou X. Vital Bleaching and Whitening Strips: Summary of Clinical Research on Effectiveness and Tolerability. Journal of Contemporary Dental Practice 2001;2:1-16.
- Dr. Paul A. Sagel, P&G Research Fellow, writing in Oral Care Science Packet
- http://www.webmd.com/oral-health/teeth-whitening
- http://www.webmd.com/oral-health/slideshow-10-secrets-to-whiter-teeth

by Visivo | Oct 8, 2019 | Uncategorized
As a parent, you understand that protecting your child’s teeth from decay and early loss is just as important as protecting their permanent teeth from the same fate.
So do dentists!
That’s why the American Academy of Pediatric Dentistry recommends placing dental sealants on the first and second set of permanent molars (those which generally come in at 6 and 12 years of age).
Your dentist might also suggest your child’s sealants be replaced – even before their permanent teeth arrive. Let’s find out why.
What are Dental Sealants?
Dental sealants are hardened plastic shields, placed on the chewing (or, “occlusal”) surface of molars and pre-molars, which seal the surface of the tooth.
Sealants work by keeping food and other bacteria-laden material from getting trapped in the tooth and causing decay — which can ultimately lead to cavities. In a study conducted by the Centers for Disease Control and Prevention, “sealants where shown to reduce decay in permanent molars by 81% approximately 2 years after placement and continue to be effective up to 4.5 years after placement.”
If you want to give your child’s molars the best protection against potential cavities, dental sealants are a great place to start.
Is it Common to Replace Sealants?
Not really. Sealants often last 15 years or more, but sometimes the need does arise.
Children who grind or clench their teeth, have a pencil or pen-biting habit, or who chew on ice and hard candy can chip or crack a sealant, necessitating its replacement. Also, tooth trauma, the type of sealant, and tooth abnormalities can affect its durability.
Here’s a great write-up from Dentistry Today about the types of sealants, failure rates and replacing sealants should you wish to learn more.